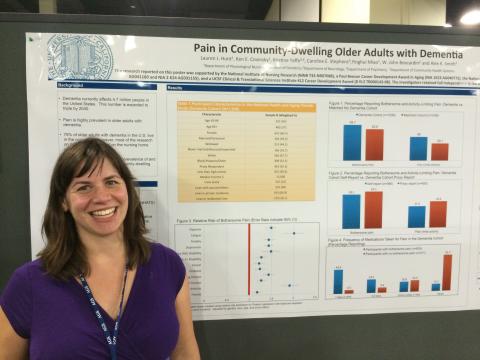
UCSF Hartford Doctoral student Lauren Hunt presented her work on "Pain in Community-Dwelling Older Adults with Dementia" at the American Geriatrics Society (AGS) in Orlando, Florida, May 16, 2014.
The AGS Annual Meeting is the premier forum for the latest information on clinical geriatrics, research on aging, and innovative models of care delivery. The meeting addresses the professional and educational needs of geriatrics professionals from all disciplines through state-of-the-art educational sessions and research presentations about emerging clinical issues, current research in geriatrics, education, health policy, and delivery of geriatric health care.
Below is information about Lauren's presentation.
Pain in Community-Dwelling Older Adults with Dementia
Lauren Hunt, MSN1, Ken Covinsky, MD MPH2,4, Kristine Yaffe, MD3,4, Caroline Stephens, PhD GNP5, Yinghui Miao, MPH4, W. John Boscardin4, PhD, Alex Smith, MD MS MPH2,4
1. Department of Physiological Nursing, UCSF; 2. Division of Geriatrics, UCSF; 3. Departments of Psychiatry and Neurology, UCSF; 4. San Francisco VAMC; 5. Department of Community Health Systems, UCSF
Key words: pain, dementia, community-dwelling
Background: A large body of science has focused on pain in persons with dementia who live in nursing homes. Little is known, however, about the prevalence and nature of pain in the 75-80% of persons with dementia who live in the community.
Methods: We analyzed data from the National Health and Aging Trends study (NHATS), a, nationally representative study of 8,245 individuals aged 65 years and older. Interviews with community-dwelling subjects were conducted in-person with self and/or proxy respondents. We used measures of cognitive function and a previously described algorithm to identify subjects with dementia. We report prevalence and national estimates of bothersome pain and pain limiting activity, as well as describe frequency of medication taken for pain. Using a multivariable regression model, we determined which factors were associated with increased risk of pain, adjusting for age, gender, race and proxy status.
Results: Of the 7,609 subjects with complete data on cognitive function, 1,038 had dementia, corresponding to 3.5 million community-dwelling people (59% age 80+, 60% female, 67% white, 42% proxy-response, 32% live alone, 16% live in residential care). 59.7% of respondents reported bothersome pain and 40.0% reported that pain limited activity. A number of comorbid conditions were associated with pain, including arthritis (adjusted Risk Ratio (ARR) 1.93; 95% Confidence Interval (CI) 1.75 – 2.12), lung disease (ARR 1.48; 95% CI 1.36 – 1.62), and heart disease (ARR 1.32; 95% CI 1.23 – 1.41). Pain was associated with requiring assistance with an Activity of Daily Living (ARR 1.29; 95% CI 1.18 – 1.42) or an Instrumental Activity of Daily Living (ARR 1.52; 95% CI 1.32 – 1.75). Depression and anxiety were also associated with higher rates of pain (ARR 1.44; 95% CI 1.34 – 1.55 and ARR 1.44; 95% CI 1.33 – 1.56), respectively. 33% of people reporting pain report rarely or never taking medication for pain.
Conclusions: Community-dwelling persons with dementia experience a high prevalence of pain. Comorbid conditions, disability, and anxiety and depression, are strongly associated with reports of pain. About 1/3 of people with pain are taking medications for pain infrequently.